Insulin Price Caps Are a Bad Idea
Cardinal Team
The Inflation Reduction Act Creates Insulin Price Caps
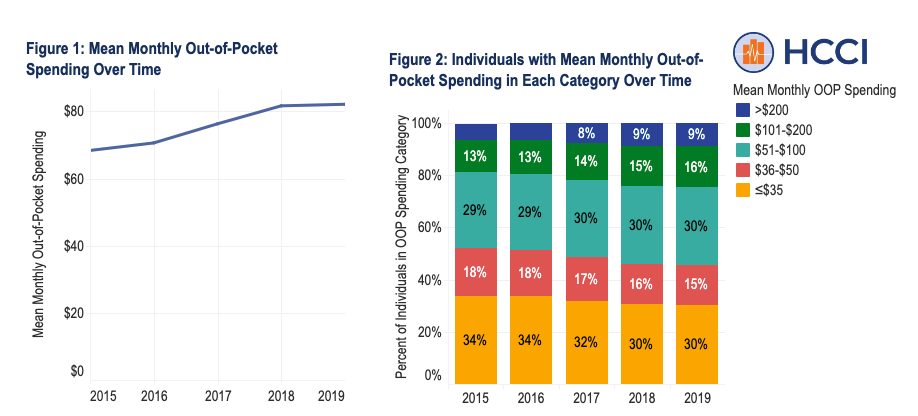
The “Inflation Reduction Act of 2022” is Washington’s latest attempt to fix problems it created. On Sunday, the Senate approved a package to combat climate change, lower healthcare costs, raise taxes, and, hopefully, reduce the federal deficit. The deal would provide for the most enormous burst of expenditures in U.S. history. Specifically, the bill would mandate private insurance companies create out-of-pocket price caps for insulin expenditures at $35/mo. However, such legislation fails to make taxpayer wallets any fuller and drastically reduces innovation capabilities in healthcare.
Swiftly after the deal passed the Senate, headlines about the vote to remove insulin price caps came to the forefront.
- Washington Post: “Republicans block cap on insulin costs for millions of patients”
- New York Times: “Republicans force the removal of a measure that would cap insulin prices at $35 for private insurers”
- Rolling Stone: “Insulin Will Remain Expensive for Many, Thanks to Republicans”
Yet, woke columnists appear to have skipped one too many ECON101 courses in undergrad. Let me walk you through it briefly.
Creating Price Caps for Insulin Hurts Health Care
There is a growing idea that the government should create ceilings for drug pricing, manufacturing, and marketing. But fundamental economics teaches that such restrictions fail to create an ethical, accessible healthcare system.
When governments create price limits on goods and services, they always initiate scarcity. When supply is low and demand is high, prices rise or, in this case, where businesses are constrained, profits must be funneled away from research and innovation. Numerous economic studies indicate price caps reduce the number of new drugs being brought into the market. Thus, temporary relief creates disastrous long-term effects.
In the last ten years, insulin prices that should have decreased naturally (i.e., supply, demand, innovation, market entrances and exits) grew rapidly.
The inflated regulation of a critical market has reduced the number of potential manufacturers, maintained high fees for insulin, and restricted accessibility. Rather than implementing price caps that are destined to fail, America should be more like Canada. (Strange, I know, but hear me out.)
How Canada Is Helping Diabetics
As it currently stands, the U.S. Food and Drug Administration imposes prescription requirements in order to access a multitude of drugs. Of course, insulin is on that list. Opposite to us, the Great White North authorizes individuals with diabetes to purchase any insulin product without a prescription. Broader access to insulin would redirect sales between consumers and manufacturers, cutting out the messy (and expensive) insurance middleman. Rather than waiting for hours to see a physician, patients would be able to obtain insulin directly from the seller. Americans have now taken matters into their own hands.
Group border-crossing trips have grown in popularity among American diabetics to obtain affordable insulin in Canada. While costs for fast acting insulin such as Humalog can be as high as $300 in the States, Canadian provinces sell the product between $30 and $45 per vial.
The caravanning to and from the nations is technically illegal, but policymakers have decriminalized it. However, the “drug smuggling,” if you will, still has limits. Despite the capability of traveling to Canada for insulin, the FDA prohibits diabetics from purchasing more than a 30-day supply.
As a result of the pandemic, Americans have become acutely aware of its healthcare system’s shortcomings. But Congress chooses to allocate its time to more government spending. To lower the cost of insulin and make it more accessible, our Washington representatives and their over-inflated bureaucracy should look in the mirror.
Jessica Dobrinsky is a Policy Analyst for the Cardinal Institute for West Virginia Policy.